Beyond Dependability - The True Essence of Trust
Trust forms the bedrock of human civilization. It's what allows us to exchange currency for goods, enter into marriages, and participate in democratic processes. While laws and contracts provide safety nets, they too ultimately rest on our trust in the institutions that enforce them. Yet when we discuss trust, particularly in professional contexts, we often reduce it to a single dimension: dependability.
The common belief that trust equates to reliability - that consistent delivery of promises automatically builds trust - oversimplifies a complex human dynamic. While dependability certainly matters, research by Frances Frei and Anne Morriss (Harvard Business Review, 2020) reveals that true trust emerges from three fundamental pillars: authenticity, logic, and empathy.
Think of dependability as the foundation - necessary but insufficient on its own. Just as a house needs more than a foundation to be habitable, trust requires more than just reliability to flourish. An individual can be perfectly dependable - meeting every commitment, fulfilling every promise - yet still fail to earn deep trust from others.
Building Healthcare Executive Competencies - A Strategic Journey (ACHE Tool)
Evidence-based research demonstrates that systematic competency development serves as the cornerstone of healthcare organizational success. The ACHE Healthcare Executive Competencies Assessment Tool (available here) provides the essential framework for this development process.
At the foundation of executive competency lies effective communication. Organizations that implement structured leadership rounds with documented learning systems consistently report significant improvements in staff engagement within six months. Beyond basic rounds, leading healthcare institutions have found success through communication laboratories that focus on real-world scenarios. These programs have demonstrated marked improvements in leader confidence, conflict resolution, and overall staff-leader communication effectiveness.
Leadership development builds naturally upon this communication foundation. The most successful healthcare organizations emphasize cross-departmental project management as a key development tool. By managing initiatives outside their primary expertise, leaders develop broader organizational understanding and enhanced collaborative capabilities. This approach pairs effectively with systematic case review programs, where actual organizational challenges become learning opportunities. Regular crisis simulation exercises round out this aspect of development, consistently improving emergency response capabilities and team coordination.
Healthcare Workforce Engagement Patterns and Indicators
The landscape of healthcare employee engagement presents a complex intersection of workforce satisfaction, patient care quality, and organizational success. At its foundation lies trust - between colleagues, between staff and leadership, and between healthcare providers and patients. Employee engagement surveys serve as crucial diagnostic tools within healthcare institutions, providing measurable insights into workforce health, organizational culture, and the strength of these trust relationships.
These surveys' significance extends beyond basic job satisfaction metrics. In healthcare environments, where patient outcomes directly correlate with staff performance, engagement surveys reveal critical patterns in care delivery quality. Evidence consistently shows that engaged healthcare workers, operating in environments of mutual trust, deliver superior patient care, maintain higher safety standards, and contribute to improved patient satisfaction scores.
Why Empathy is Non-Negotiable for Building Trust in Leadership
Leadership in the modern workplace requires more than just strategic thinking and technical expertise. At its core, effective leadership demands a quality that cannot be learned from textbooks or acquired through experience alone: empathy. The ability to understand, share, and respond to the feelings of others has become the cornerstone of building trust within organizations, and its absence can create irreparable rifts between leaders and their teams.
Trust forms the foundation of all meaningful workplace relationships. It's the invisible thread that weaves teams together, enables innovation, and drives organizational success. Yet trust itself is built upon something even more fundamental: the capacity for empathy. When leaders demonstrate genuine empathy, they create an environment where trust can flourish naturally. This connection between empathy and trust isn't coincidental—it's essential to human psychology and social dynamics.
The Heart of Physician Recruitment - Creating Value, Voice, and Community
The story of physician recruitment is fundamentally a human one. It's a story about professionals who have dedicated their lives to healing, seeking not just a place to practice, but a place to belong. It's about organizations learning to create environments where these healers can thrive, contribute, and find fulfillment in their calling.
The journey of physician recruitment begins long before the first interview. It starts with the understanding that physicians seek more than competitive compensation and state-of-the-art facilities. They seek a voice in their practice environment, a seat at the decision-making table, and a culture that values their expertise beyond clinical skills.
Many physicians can recall moments when they felt like mere cogs in a healthcare machine – their insights overlooked, their concerns dismissed, their professional growth stagnated. These experiences shape what they seek in their next role: an environment where their voice matters, where their contributions are valued, and where they can shape the future of patient care.
Analyzing Minnesota's Regulatory “Moat” and Wisconsin's “Free Market Approach”
When it comes to healthcare facility expansion, Minnesota and Wisconsin represent two distinct regulatory philosophies. Minnesota's Certificate of Need (CON) requirements create what many healthcare analysts describe as a protective "moat" around existing healthcare facilities, while Wisconsin's free-market approach since 2000 has opened the doors to unrestricted expansion. Both approaches carry significant implications for healthcare providers, patients, and market dynamics.
The Power of Vulnerable Leadership
Many believe leadership assumes or means leaders have all the answers. Like many executives, I thought showing vulnerability would undermine my authority and effectiveness as a leader. However, a powerful insight from Brené Brown's research shows an entirely different perspective: connection—the very thing we seek as leaders—requires vulnerability.
Think about the leaders who've most influenced your life. Chances are, they weren't the ones who maintained a perfect facade. They were the ones who showed up authentically, who admitted when they didn't have all the answers, and who shared their challenges alongside their victories. These leaders understood something fundamental about human nature: we connect through our shared humanity, not our pretense of perfection.
Mental Health Care Access in Rural America
Across rural America, a critical healthcare crisis is unfolding in plain sight. In thousands of communities far from major cities, millions of Americans face a troubling paradox: their areas have some of the highest needs for mental health support yet the fewest resources to address these challenges. The impact touches every segment of rural society, from working adults to seniors, teenagers to young children., where mental health services are critically underrepresented despite growing needs. In the vast expanses between major cities, millions of Americans face a troubling paradox: their communities often have the highest need for mental health support yet the fewest resources to address these challenges.
The scope of this rural mental health crisis is staggering. More than 60% of rural Americans live in areas designated as Mental Health Professional Shortage Areas. This shortage translates into real human impact – rural residents experience higher rates of depression, substance abuse, and suicide than their urban counterparts. The suicide rate in rural areas is one and a half times higher than in urban communities, a statistic that reflects the urgent need for better mental health resources.
Understanding Just Culture - Building a Foundation for Patient Safety
Where lives hang in the balance and split-second decisions can make all the difference, creating a safe environment isn't just about rules and regulations—it's about culture. Specifically, it's about fostering what healthcare experts call a "Just Culture," a framework revolutionizing how healthcare organizations approach patient safety and staff accountability.
At its heart, Just Culture represents a fundamental shift in our thinking about mistakes and accountability in healthcare settings. Rather than defaulting to blame when things go wrong, this approach encourages organizations to take a deeper look at both individual and systemic factors that contribute to errors. It's about finding the delicate balance between personal responsibility and organizational support—understanding that while healthcare professionals must be accountable for their choices, they also deserve support when systems fail them.
Building Better Products and Services Through Healthy Conflict
Many organizations still struggle with one of the most powerful catalysts for growth: productive disagreement. The instinct to avoid conflict, while natural, often leads to missed opportunities and stagnant thinking. But when handled skillfully, disagreement becomes a driving force for better products, services, and organizational outcomes.
Research from Harvard Business School professor Amy Edmondson reveals a counterintuitive truth: teams that perform at the highest levels often experience the most constructive disagreement. This finding challenges the common belief that harmony equals productivity. Instead, it suggests that our ability to disagree respectfully and productively may be the key to unlocking innovation and excellence.
Center of Excellence Certification as a Differentiator
Standing out and creating a competitive advantage in the marketplace while delivering exceptional patient care has become more challenging than ever. Healthcare organizations continually search for ways to differentiate themselves meaningfully in their markets. One powerful approach that is gaining traction is pursuing Center of Excellence certification through leading accrediting bodies such as DNV GL Healthcare and The Joint Commission (TJC). While each accrediting organization has its unique approach, the strategic value of these certifications extends far beyond the credential itself.
When viewed through the lens of Michael Porter's competitive strategy framework, an orthopedic center of excellence certification emerges as a powerful tool for creating sustainable competitive advantage. Whether through DNV GL Healthcare's innovative ISO 9001-based approach, The Joint Commission's disease-specific care certification, or other recognized programs, the certification process doesn't just validate clinical excellence – it serves as a catalyst for comprehensive organizational transformation that can reshape market positioning and operational effectiveness.
Why Job Transitions Are So Challenging — and How We Can Navigate Them
Not long ago, I found myself facing an unexpected job transition. It was a shift I hadn’t planned for, and it has brought with it a complex mix of emotions—some I expected, others I didn’t. Moving out of a role I’d known well, even without a new position lined up, carries both excitement and apprehension. I realized that this transition was not just about finding a new job; it was an invitation to pause and reflect on where I’ve been, where I want to go, and what truly matters to me in my career.
Going through this experience has made me deeply appreciate the power of reflection and the value of support during a job transition. Many of us will face these changes, yet they’re rarely easy. Today’s professional landscape doesn’t offer the clear, structured paths it once did. Instead, we often have to define our own milestones, successes, and markers of progress, relying on our networks—our friends, mentors, and colleagues—to help us fill in the gaps. As I continue to navigate this phase, I’ve realized that one of the most meaningful ways we can move through job transitions is by reflecting on our journey and supporting one another.
Boosting Employee Engagement in Healthcare: Strategies for Responding to Metrics That Need Improvement
Employee engagement in healthcare isn’t just a buzzword—it’s a vital component of delivering high-quality patient care and maintaining a thriving organization. However, understanding and responding to engagement metrics that reveal areas of concern can be challenging. In this post, we’ll explore how to interpret these metrics effectively and take meaningful action to create a positive, supportive environment for healthcare professionals.
Building Trust and Connection - The Power of CICARE in Patient Interactions
During my early years as a Certified Nursing Assistant (CNA) in a long-term care facility, I was introduced to a simple yet transformative concept by the director of nursing. It wasn’t formally known as CICARE at the time, but its principles stayed with me throughout my entire career in healthcare. The director of nursing emphasized the importance of how we engage with patients and their families, stressing that a compassionate introduction sets the tone for the entire interaction. Reflecting on this experience, I realize how foundational this lesson was and how it resonates with the CICARE protocol used in many healthcare organizations today.
Merging Organizational Pillars for Overall Success: One Great Experience – One Great Team
People choose healthcare as a career because it fulfills their individual sense of purpose. It is passion driven. Consumers select their healthcare provider because they feel a real sense of concern and dedication from those professional providing the care. It is the combination of these feelings and desires that creates the basis of a great culture within an organization. In a practical sense, it is the coming together of two major strategic approaches into organizational goals: one great experience - one great team.
Physician Recruiting: How Culture Sets Your Organization Apart
Physician recruiting in the healthcare environment remains more competitive than ever. While compensation and benefits remain important, culture is emerging as a key differentiator for organizations seeking to attract and retain top physician talent. The physicians I’ve spoken with describe a common theme: beyond pay and career growth, they want to feel valued and have a voice in shaping their practice. Many have experienced what they describe as a “treadmill” environment, where they were seen merely as "producers," leading to burnout and disengagement.
Managing People, Process, and Plan - A Systematic Approach to Organizational Success
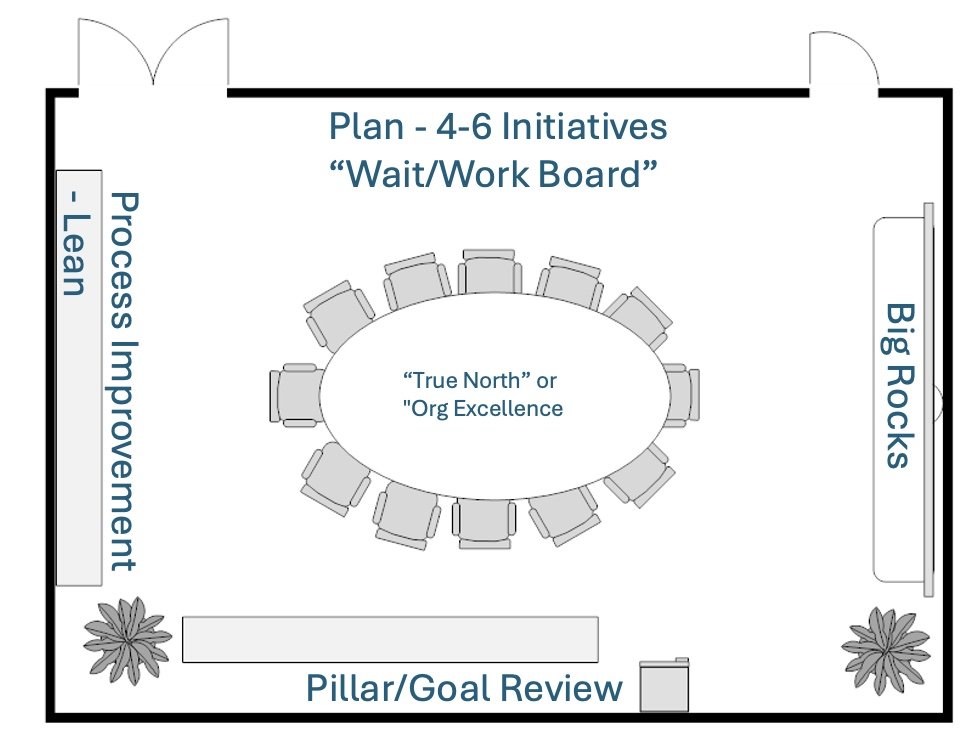
In many healthcare organizations, the key to achieving success lies in effectively managing People, Process, and Plan. To truly harness this triad, it requires a disciplined, structured approach that keeps the entire team aligned with the organization’s mission, strategic goals, and improvement initiatives. One highly effective method for maintaining this alignment and keeping progress on track is what I call the "Around-the-Room Review."
This blog will explore how to set up a structured review process by utilizing the physical layout of a room to track progress and address key strategic priorities in a systematic way.
Creating Synergy Between People and Process: Using Lean to Improve Emergency Department Efficiency and Patient Experience
Emergency departments (EDs) are a pivotal point of entry for patients requiring urgent medical attention, making ED efficiency a critical metric for hospitals. The Centers for Medicare & Medicaid Services (CMS) developed several performance measures to track how well hospitals manage patient flow, including the measure OP-18b: the median time from emergency department arrival to emergency department departure for discharged patients. This measure, while commonly used as a benchmark for time-based performance, is more than just a number. It reveals opportunities for improving patient flow, reducing bottlenecks, and enhancing overall patient experience through effective teamwork and process optimization.
By leveraging Lean Process Improvement principles, hospitals can reduce inefficiencies and enhance coordination between departments, allowing patients to move more seamlessly through the emergency department. But achieving these results requires more than just good processes—it requires a synergy between the people working at the front lines of patient care and the processes designed to streamline their work. This article explores how a thoughtful combination of “People” and “Process” can help hospitals not only meet the CMS OP-18b standard but also significantly improve the quality of care and the patient experience.
Measuring Success Through Strategic Pillars
Delivering sustainable results requires more than just setting broad organizational targets. It’s about creating a system where every aspect of the organization, from leadership to individual departments, aligns its efforts with a unified purpose. To accomplish this, I propose using a “Pillar” framework by which we measure the success of our efforts across the critical areas of People, Process, and Plan (Employee Engagement/Culture, Lean Process Improvement, and Strategy).
These strategic pillars - Quality, Workforce, Patient Satisfaction, Finance, and Community - serve as foundational guides that shape our future. Each pillar will have overarching organizational goals that cascade down to specific departmental objectives, creating a cohesive framework where every hospital department plays an active role in achieving the organization’s mission.