Leveling the Playing Field to Close the $40 Million Gap Threatening Rural Hospital Districts
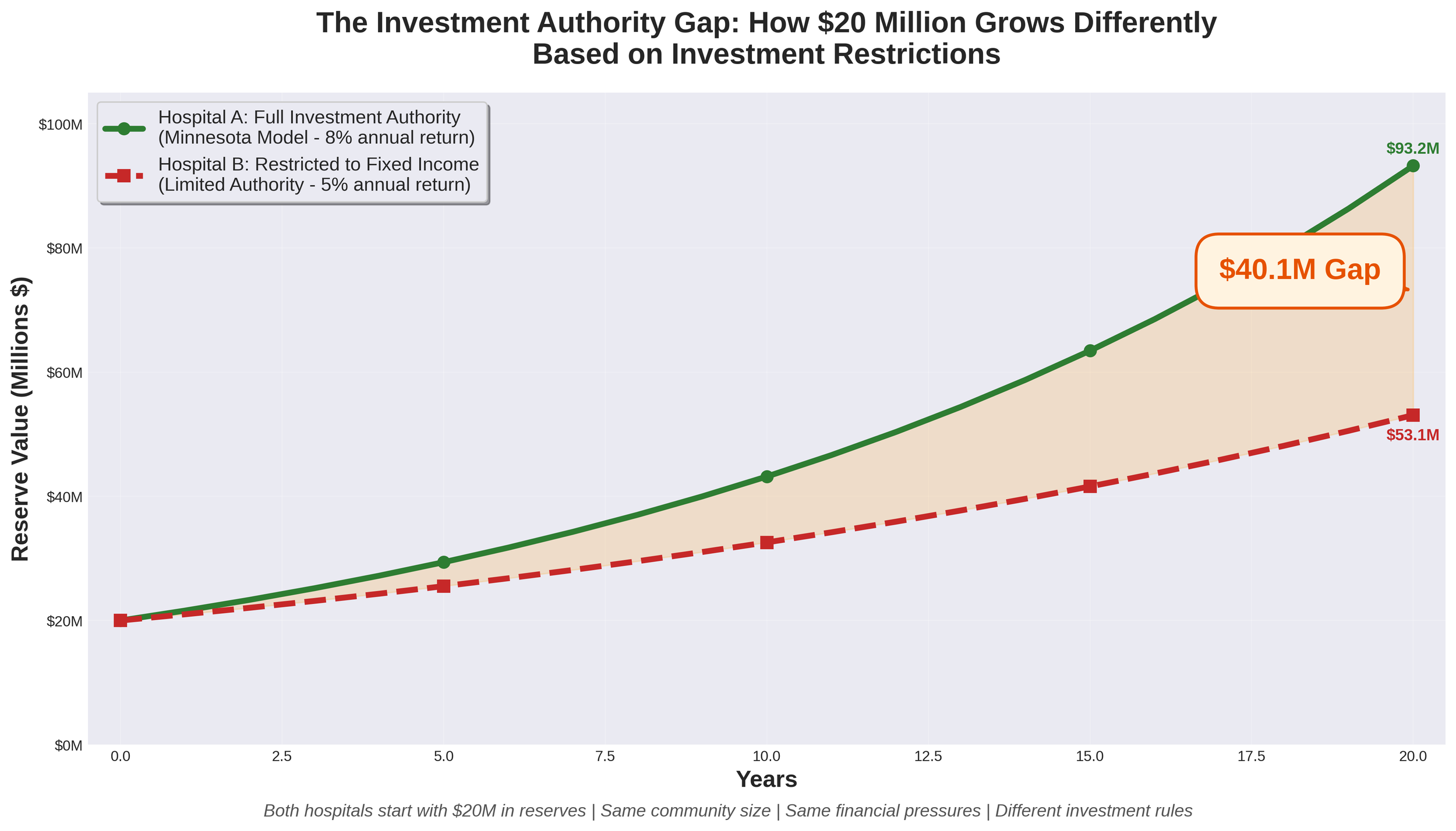
Imagine two nearly identical Critical Access Hospitals in neighboring states. Both serve rural communities of approximately 11,000 residents. Both have worked hard to build $20 million in reserves to weather financial storms and invest in their futures. Both face the same financial headwinds threatening rural healthcare nationwide.
There's just one critical difference: One hospital can invest its reserves like every other non-profit healthcare organization in America. The other cannot.
Twenty years later, the first hospital has grown its reserves to approximately $93.2 million. The second hospital has barely $53.1 million. That $40 million gap represents the difference between survival and closure for a rural community.
Rural hospitals across America are facing unprecedented financial pressures. More than 180 rural hospitals have closed nationwide since 2005, and the trend is accelerating. The challenges are well-documented: Medicare and Medicaid reimbursement rates that don't cover the cost of care, rising levels of uncompensated care as insurance coverage gaps widen, workforce shortages requiring premium compensation to recruit and retain staff, healthcare-specific inflation that outpaces general inflation (particularly for labor, pharmaceuticals, and supplies), escalating technology and cybersecurity costs, and increasing regulatory demands.
For hospital districts across many states, these universal challenges are compounded by a structural disadvantage that few people understand: constitutional or statutory restrictions that prevent them from competing on a level playing field with private non-profit hospitals. While private 501(c)(3) hospitals can invest their reserves in diversified portfolios including equities, many governmental hospital districts remain restricted to low-return fixed-income investments. This gap in investment authority creates a compounding disadvantage that threatens the long-term viability of publicly-owned rural hospitals.
Let's examine this issue using Nebraska as a case study—but the implications extend to hospital districts in any state facing similar investment restrictions.
An Open Letter to Tyson Foods Leadership
My name is Jason Douglas, and I serve as CEO of Lexington Regional Health Center, a Nebraska Hospital District, here in Lexington, Nebraska. I came to this community in March of this year as a healthcare administrator who passionately believes in the mission of serving rural communities. I'm writing to you as someone who has spent the past two weeks watching families in our community try to find their footing after your November 21st announcement.
You gave them a Friday afternoon, right before Thanksgiving. It'll be memorable, as November 21st just happened to be my birthday. I'd planned to spend it settling further into this community I'd grown to love and appreciate in my short time here. Instead, I spent it fielding calls and beginning to understand the scope of what your decision would mean for the people I came here to serve.
What matters is that 3,200 people learned that same day their jobs would be gone by January 20th—then went home to prepare a holiday meal with their families. To sit across the table from their children and try to find something to be thankful for. To lie awake that night doing math in their heads—how many paychecks left, how long until insurance runs out, whether they can make rent in February.
That was your timing. That was your choice.
2025 Rural Healthcare Year in Review - When Rhetoric Met Reality
The year 2025 will be remembered as the moment rural healthcare advocates learned to read between the lines of political theater. It began with Robert F. Kennedy Jr.'s confirmation hearings for HHS Secretary, where nearly every senator—Republican and Democrat alike—stressed the critical importance of preserving healthcare access and coverage in rural America. It ended with rural hospitals facing the largest federal healthcare cuts in Medicaid's history, a marketplace subsidy cliff that may never be resolved, and a "transformation grant" that delivers a fraction of what the rhetoric promised.
The question we must ask: Do the policies enacted in 2025 support the narrative presented during Kennedy's confirmation, or do they expose it as empty posturing?
The $100,000 H-1B Fee - A Policy That Undermines American Competitiveness
The recent decision to impose a $100,000 fee on new H-1B visa applications represents a fundamental misunderstanding of how global talent drives American economic success. While framed as protecting American workers, this policy will likely harm both American competitiveness and the very workers it claims to help.
America's dominance in technology, healthcare, and innovation has been built on a simple principle: attract the world's best talent and let them create value here. This policy abandons that winning strategy for a fundamentally flawed premise that high-skilled immigration is a zero-sum game. The $100,000 fee effectively transforms H-1B visas from a workforce tool into a luxury good. For a medical resident earning $55,000 annually, no hospital will rationally pay twice their salary just for the privilege of hiring them. For a brilliant recent PhD who might revolutionize artificial intelligence or develop life-saving treatments, the fee creates an arbitrary barrier that has nothing to do with their potential contribution to America.
Strengthening Rural Healthcare - Understanding the Nebraska High Value Network and Value-Based Care
On June 5, 2025, the Nebraska High Value Network (NHVN) officially launched with 19 critical-access hospitals joining forces to strengthen healthcare delivery across rural communities. This collaborative network, organized by Cibolo Health, represents more than just a partnership—it's a strategic approach to ensuring sustainable, high-quality healthcare remains accessible in rural Nebraska.
The network's cornerstone is a clinically integrated network (CIN) that will serve nearly 300,000 patients while allowing each hospital to maintain its independence and community focus. For healthcare leaders like myself, this model offers a compelling path forward in an increasingly complex healthcare landscape.
The Future of Medicine - How AI and Quantum Computing Are Revolutionizing Drug Discovery and Patient Care
We stand at the threshold of a medical revolution. While the promise of personalized medicine has tantalized researchers for decades, we're finally seeing the convergence of technologies that can deliver on that promise at scale. Leading this charge is an unlikely partnership between a century-old Danish pharmaceutical company and cutting-edge quantum computing research—a collaboration that's rewriting the rules of drug discovery and patient care.
Novo Nordisk, best known for its diabetes treatments and the blockbuster obesity drug Wegovy, has quietly become one of the most innovative forces in computational medicine. Their recent breakthroughs offer a glimpse into a future where artificial intelligence doesn't just assist doctors—it fundamentally transforms how we understand, predict, and treat disease.
Leadership Perspectives - Navigating the Nuances of Authority and Influence
We're excited to welcome Jess Nuutinen back to our leadership series with her insightful exploration of the critical distinction between being a boss and being a leader. Following her previous contribution on shared governance, Jess now turns her analytical lens to the subtle yet profound differences that separate positional authority from true leadership. In "Boss vs. Leader: Understanding the Key Differences," she skillfully dissects how these contrasting approaches affect team dynamics, organizational culture, and long-term success. Jess's thoughtful examination of authority versus influence, task-orientation versus people-orientation, and control versus empowerment provides valuable guidance for healthcare professionals at every level. Her practical wisdom reminds us that effective leadership transcends titles and hierarchies—a timely message that complements our growing collection of leadership perspectives. As you read her compelling analysis, we invite you to reflect on your own leadership style and consider how you might incorporate more leadership qualities into your daily practice.
Transformative Leadership - Making a Meaningful Difference
We're pleased to continue our leadership series with an enlightening contribution from Dan Swenson that challenges conventional notions of leadership. In "Transformative Leadership - Making a Meaningful Difference," Dan thoughtfully explores how true leadership transcends formal titles and hierarchies to focus on creating genuine impact. His perspective offers a refreshing counterpoint to authority-centric leadership models, emphasizing instead how service, compassion, and humility form the foundation of transformative leadership. Dan's insights are particularly relevant in healthcare settings, where leadership decisions directly affect patient outcomes and organizational culture. As Frontier Strategy Partners continues to showcase diverse leadership philosophies, Dan's emphasis on accessible leadership—available to everyone regardless of position—adds a valuable dimension to our ongoing conversation. His message that leadership is ultimately measured by positive impact rather than power aligns perfectly with our commitment to exploring leadership approaches that create lasting, meaningful change.
Building Excellence in Healthcare Through a Comprehensive Management System
Exceptional performance is rarely achieved through isolated initiatives or the heroic efforts of individuals. Instead, sustainable excellence requires a comprehensive management system that aligns people, processes, and strategic direction. Having observed this healthcare transformation effort, I've become convinced that the "three-legged stool" approach—integrating People, Process, and Plan—offers a powerful framework for healthcare organizations seeking to elevate performance across all dimensions.
Leadership Perspectives - The Critical Role of Non-Clinical Leadership in Healthcare Excellence
We're excited to continue our leadership series with a compelling contribution from Kevin Stranberg of Stranberg and Associates. In this insightful piece, Kevin illuminates the often-overlooked yet essential role that non-clinical leadership plays in creating exceptional healthcare experiences. Building upon the shared governance principles explored in Jess Nuutinen's previous article, Kevin expertly demonstrates how non-clinical departments form crucial pillars in a healthcare organization's cultural foundation. His holistic perspective reminds us that exceptional patient care depends on every team member—from registration to housekeeping—working in concert toward a common mission. Kevin's thoughtful analysis of empowerment, collaboration, and accountability across departmental boundaries reflects his deep understanding of healthcare systems and organizational dynamics. We're confident his wisdom will provide valuable insights for leaders throughout your organization, regardless of their clinical or non-clinical roles.
Strong leadership in non-clinical departments of the healthcare system is essential to overall success. Although most clinical departments generally have limited direct contact with patients, their efforts are important components of the overall culture of the organization. Time and time again when patients are asked the question “did staff work together to care for you?” they include everyone they have come in contact with during their visit – registration, housekeeping, nutrition, patient financial to name a few. As a leader of non-clinical staff, the focus of the work needs to be clear and important to every staff. This focus centers on many of the same priorities listed by Jessica Nuutinen in the previous leadership article on Shared Governance – Empowering Healthcare Teams Through Collaborative Leadership for clinical staff leadership.
Shared Governance - Empowering Healthcare Teams Through Collaborative Leadership
In our continuing leadership blog series, we're pleased to feature Jess Nuutinen's insightful exploration of shared governance—a cornerstone concept in modern healthcare leadership. Jess brings a wealth of experience to this topic, offering a thoughtful analysis of how collaborative decision-making transforms healthcare organizations. As Frontier Strategy Partners continues to examine diverse leadership approaches, Jess's perspective highlights how distributing authority and responsibility across all levels of healthcare professionals creates more resilient, innovative, and patient-centered organizations. Her practical framework for implementing shared governance reflects our commitment to providing actionable leadership strategies that can be applied across various healthcare settings. Join us as Jess illuminates this powerful approach that bridges the gap between frontline caregivers and organizational leadership.
Shared governance is a vital framework in health care and nursing that promotes collaboration, accountability, and empowerment among nursing staff and other health care professionals. By fostering a participative decision-making process, shared governance allows nurses to have an active role in shaping policies, procedures, and practices that directly impact patient care and workplace dynamics.
The A3 Approach - A Practical Guide to Strategic Documentation in Healthcare
Organizations face unprecedented challenges that demand focused strategic responses. Yet many healthcare institutions struggle with strategic clarity—developing plans that are unwieldy, difficult to communicate, and even harder to implement effectively. The A3 methodology offers a powerful solution to this common challenge.
Originally developed by Toyota as part of their lean management system, the A3 approach has found remarkable resonance in healthcare settings. Taking its name from the international paper size (11x17 inches) that serves as its canvas, this methodology constrains strategic documentation to a single page—forcing clarity, precision, and prioritization.
Measuring Success Through Strategic Pillars
Delivering sustainable results requires more than just setting broad organizational targets. True success comes from creating a comprehensive system where every aspect of the hospital, from executive leadership to individual departments, aligns its efforts with a unified purpose. At the heart of this alignment lies a structured approach to goal setting that ensures the organization moves forward cohesively toward its mission and vision.
The strategic pillar framework offers healthcare organizations a powerful methodology to measure success across critical operational areas. By organizing goals around five foundational pillars—Quality, Workforce, Patient Satisfaction, Finance, and Community—hospitals create clear pathways for improvement while ensuring that priorities cascade effectively throughout all levels of the organization.
The Strategic Impact of Communication on Organizational Success
Communication stands as the foundational element that shapes organizational culture and drives employee engagement. Far beyond the simple exchange of information, strategic communication serves as the invisible architecture that aligns teams, builds trust, and propels organizations toward their goals.
Successful organizational communication hinges on three critical dimensions: the message content, the delivery mode, and the target audience. When these elements are strategically aligned, communication transforms from a mundane operational function into a powerful catalyst for organizational cohesion and performance.
“Essential Leadership Tools”
We're delighted to launch our leadership blog series featuring unique insights from across our talented team at Frontier Strategy Partners. Craig Saylor kicks off the series with his thought-provoking piece on "Essential Leadership Tools" - a compelling exploration of intentional leadership practices that challenge conventional approaches. Drawing from his extensive experience, Craig offers valuable perspectives on mission-driven leadership, fact-based decision-making, team empowerment, and achieving meaningful work-life balance. His practical wisdom sets the perfect tone for this series, demonstrating the caliber of insights you can expect in the weeks ahead. Craig's ability to distill complex leadership principles into actionable strategies exemplifies why he's such a valued voice in our organization and the healthcare leadership community. We hope you'll find his observations as inspiring and applicable as we do.
The Physician Journey - From Recruitment to Meaningful Partnership
Physician recruitment has become more than a matter of filling positions—it's about creating meaningful connections between talented healers and the communities they serve.
At its core, physician recruitment tells a deeply human story. It's about professionals who have dedicated their lives to healing, searching not just for a place to practice, but a place to belong. Healthcare organizations must recognize that beyond competitive salaries and cutting-edge facilities, physicians seek environments where they can make meaningful contributions, grow professionally, and find fulfillment in their calling.
Many physicians carry memories of environments where they were “put on a high-speed treadmill and forgotten” (actual quote from a previous Physician I recruited regarding the culture of his/her prior employment)—their insights overlooked, their concerns minimized, their growth stunted. These experiences profoundly shape what they seek in new opportunities: workplaces where their voices matter, their expertise is valued beyond clinical skills, and they can actively shape the future of patient care.
My First Week in Lexington - Pride, Gratitude, and Possibility
It's been just short of one week since we crossed the Nebraska state line, greeted by those familiar words: "Nebraska - the good life." After several days immersed in this community, I can confirm that simple phrase holds even more meaning than I anticipated. It's not just a slogan on a highway sign, but a lived reality of the community we've joined, the life we're building, and the good we're already beginning to do together.
During my interview process, I found myself looking up in Lexington High School's cafeteria where 46 flags hang, each representing a different nation, each telling a story of journey and belonging. Now, after a week of meeting the people those flags represent, I'm even more moved by what this symbolizes. These aren't just decorations—they're declarations of a community that has chosen to celebrate its diversity rather than be divided by it.
Emotional Intelligence - Advanced Strategies for Workplace Success
Emotional intelligence (EI) continues to be recognized as a cornerstone of professional success in today's complex workplace. Since our previous exploration of EI assessment tools, the landscape of work has evolved significantly, presenting new challenges and opportunities for applying emotional intelligence principles. This updated perspective aims to deepen your understanding of how emotional intelligence can be leveraged for both personal growth and team development in contemporary work environments.
The Transformative Power of Professional Coaching - How External Perspectives Drive Excellence
Many of us reach a plateau in our careers where improvement seems to stall. Despite our best efforts, we may find ourselves unable to identify the barriers holding us back or the specific changes needed to overcome them. This phenomenon is precisely what renowned surgeon and public health innovator Dr. Atul Gawande explores in his insightful presentation on the profound impact of professional coaching.
Dr. Gawande shares a compelling personal narrative about his journey as a surgeon who, after years of practice, found his improvement curve flattening. Like many accomplished professionals, he initially experienced steady progress in his early career, watching his complication rates drop year after year. But after about five years, this improvement plateaued, leading him to question: "Is this as good as I'm going to get?"
What follows is a remarkable testament to the power of external perspective. Dr. Gawande invited a retired professor to observe his surgical technique—a practice uncommon in his field but standard in others like music and sports. Despite believing his performance was flawless, he received a page full of observations about small but significant details he had missed: suboptimal lighting, improper elbow positioning, and other subtle inefficiencies that affected his performance.
The “Strategic Parking Lot” - Managing Future Initiatives While Maintaining Focus
Organizations face a constant stream of new ideas, opportunities, and potential projects. While innovation and forward thinking are essential for growth, attempting to pursue too many initiatives simultaneously often leads to diminished results across the board. This creates a fundamental tension: how can organizations maintain laser focus on current strategic priorities while ensuring valuable future opportunities aren't lost?
Most organizations have a set of primary initiatives that demand significant resources, executive attention, and cross-functional collaboration. These initiatives typically represent the organization's most important strategic priorities and require sustained focus to execute successfully. However, during the execution of these critical initiatives, new ideas continuously emerge. Some arise from market changes, others from customer feedback, and still others from internal innovation. Each may hold tremendous potential value, yet adding them to an already full plate risks diluting focus and compromising overall execution.